Wednesday, January 21, 2026

MEDICALLY REVIEWED BY
Andrada Costache, MD
Dr. Costache is a radiologist with over 10 years of experience. She specializes in thoracic radiology.

For years, PACS (Picture Archiving and Communication System) was defined simply as "digital film." If it replaced the file room, it was a success.
But in the modern healthcare environment, that definition is obsolete. Today, a PACS is the Enterprise Operating System for imaging. It must do more than store images; it must orchestrate workflows, integrate with the EMR via modern standards, and defend against ransomware.
PACS connects acquisition, DICOM storage, diagnostic viewing, RIS worklists, and EHR context into one operational layer.
If you are evaluating a new PACS, you cannot rely on definitions from 2010. This guide breaks down the three layers that define a high-performance system in 2026.
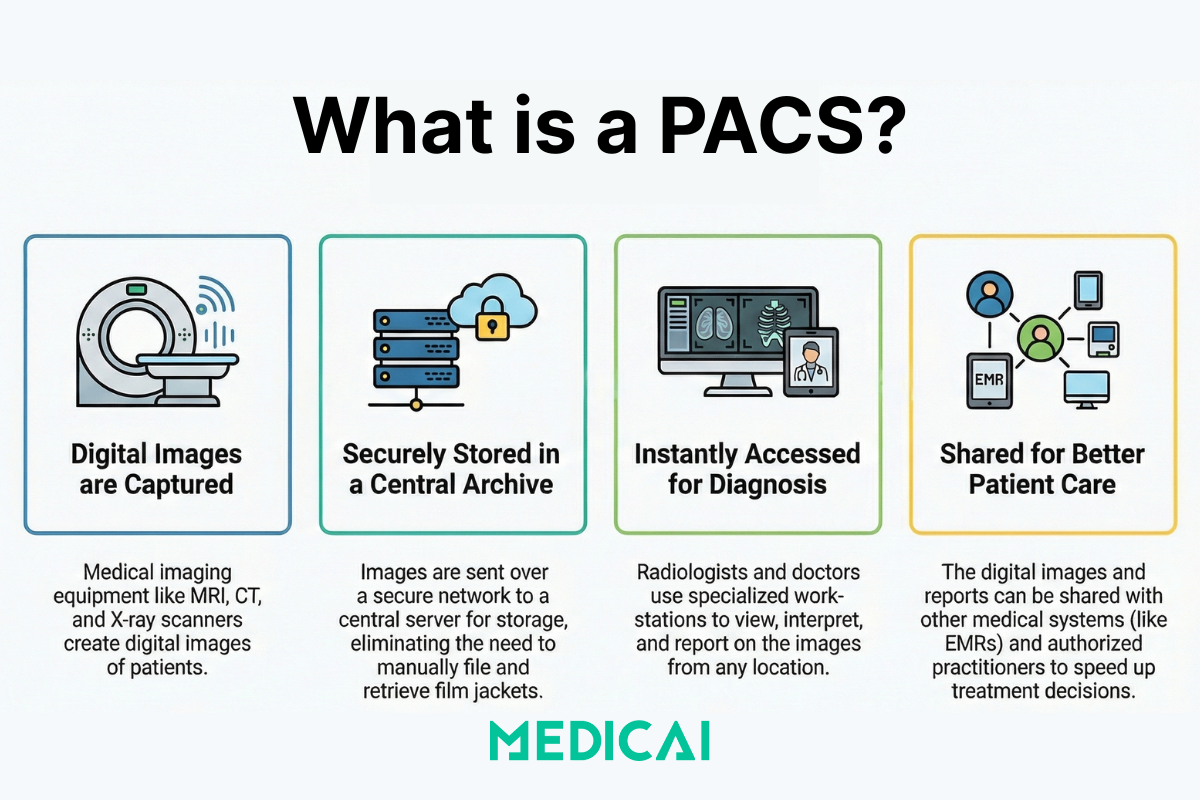
PACS stands for Picture Archiving and Communication System. It is a medical imaging technology used by hospitals and clinics to securely store, retrieve, manage, and share digital images produced by modalities like X-ray, CT, MRI, and Ultrasound.
At its simplest level, a PACS works by replacing physical film archives with a digital database. It consists of four key components:
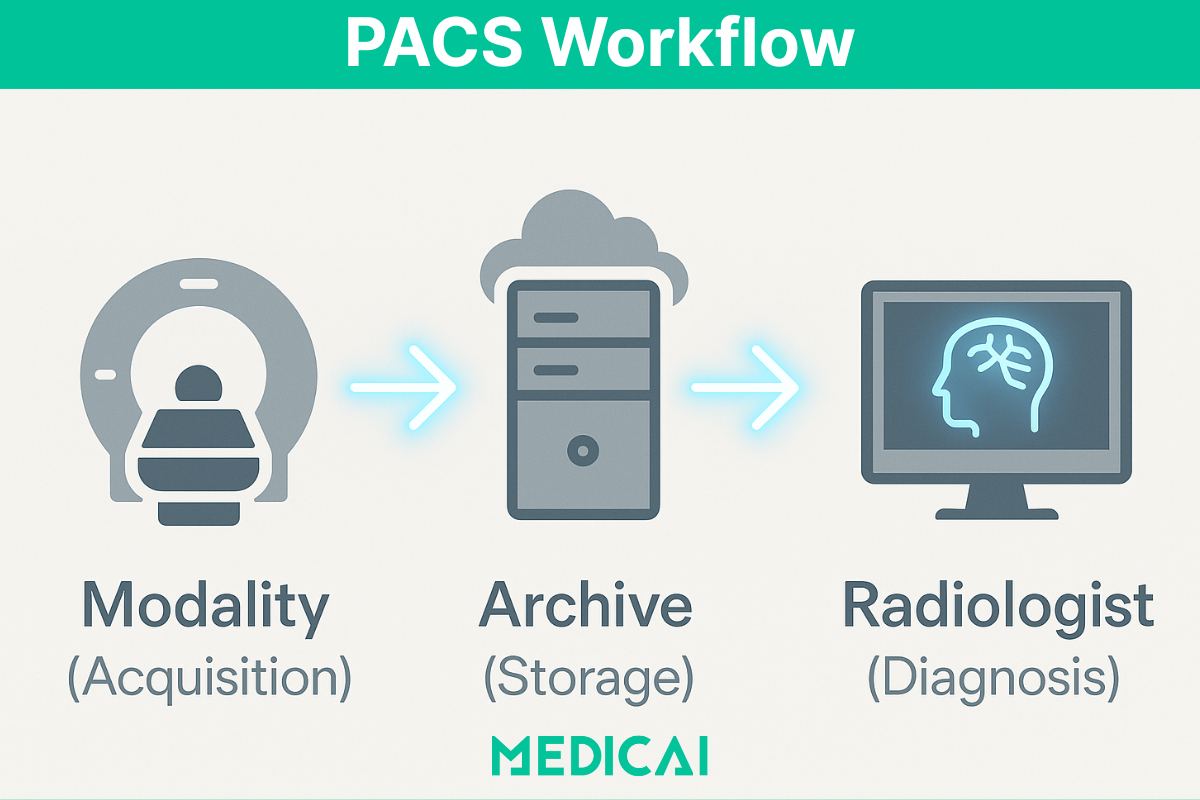
PACS workflow follows the clinical loop, order to report. PACS workflow starts when an exam is ordered, scheduled, and placed on a modality worklist. PACS workflow continues when the modality acquires images and sends DICOM objects to the archive. PACS workflow continues when radiologists read the study, compare priors, and sign a report. PACS workflow ends when images and results reach the referring team and the EHR. IHE Scheduled Workflow exists to keep this loop consistent across HIS, RIS, modalities, PACS, and reporting systems.
.avif)
Medical image storage relies on a physical local server located in the hospital basement. While this offers speed, it creates data silos. A modern PACS system replaces this rigid infrastructure with a flexible Hybrid Edge Architecture.
Instead of simply acting as a hard drive, the system utilizes a Vendor Neutral Archive (VNA) core. This means that unlike legacy PACS software that locks your data in proprietary formats, your patient data is stored in standard DICOM native format.
PACS manages clinical workflows and viewing, VNA manages long-term, vendor-neutral storage and migration independence, and many enterprises run both.
This PACS architecture ensures true data sovereignty while allowing the cloud PACS to scale instantly using geo-redundant cloud storage protocols, protecting you from ransomware and hardware failure.
PACS data lifecycle management decides what stays hot, what moves to archive, and what retention rules govern storage. PACS retention periods vary widely across jurisdictions and care settings, and published reviews report storage duration ranges measured in months to years.
PACS lifecycle planning includes migration windows, index rebuild time, and metadata integrity checks. PACS lifecycle planning reduces long-term cost because older studies are rarely accessed, but legal and clinical requirements still demand availability.
Viewing medical images required installing heavy software on a specific workstation in the hospital. If a doctor wanted to access images from home, they had to struggle with slow VPNs. Modern PACS solutions utilize HTML5 Zero-Footprint Viewers to eliminate this bottleneck.
This technology changes the physics of image retrieval. Instead of downloading the entire file to the device (client-side), the system uses Server-Side Rendering (SSR). The cloud server processes the heavy data—like massive 3D Tomosynthesis volumes or Cardiac CINE loops—and streams a high-definition interactive video feed to the web browser.
PACS performance depends on priors availability. PACS prefetch workflows pull relevant prior studies before the radiologist opens the current study. DICOM prefetch gets described as a workflow automation mechanism for fetching relevant priors from image archives such as PACS and VNA.
PACS prefetch reduces wasted reading time and reduces repeat queries during peak hours.
Now, a radiologist can perform diagnostic viewing on a laptop or tablet with zero latency, accessing the same advanced tools found on a dedicated diagnostic workstation, such as Multi-Planar Reconstruction (MPR) and Maximum Intensity Projection (MIP), without waiting for data to buffer.
A standalone PACS system creates data silos. To be effective, it must integrate with other systems like your Electronic Health Record (EHR) and Radiology Information System (RIS). Legacy platforms often rely on outdated point-to-point connections, but Medicai utilizes a modern API-first architecture built on HL7 FHIR standards.
This allows for true bi-directional PACS integration. When a doctor updates patient history in the EHR, the metadata is instantly synchronized with the imaging file. Unlike basic AI tools that simply flag potential issues, our platform acts as an AI Orchestration Engine. It routes specific studies to third-party algorithms for automated triage—prioritizing critical cases like strokes—and embeds the findings directly into the DICOM Structured Report (SR).
This means doctors don't just get a "second opinion" from the computer; they get a fully automated, data-driven workflow that reduces manual data entry and speeds up diagnosis.
PACS interoperability relies on two transport families, DICOM DIMSE and DICOMweb. DICOM DIMSE covers classic store, query, and retrieve operations used by modalities and legacy archives. DICOM Query/Retrieve commonly uses C-FIND for search and C-MOVE for retrieval routing.
DICOMweb covers web-native access for modern viewers and integrations. DICOMweb services include REST patterns for query, retrieve, and store, which map to workflows like QIDO-RS, WADO-RS, and STOW-RS.
PACS integration keeps using HL7 v2 in many hospitals, and PACS integration uses FHIR more often for API-first data exchange.
Healthcare professionals often confuse the two. Here is the distinction between DICOM vs PACS:
Analogy: If DICOM is the "PDF" format, PACS is "Adobe Acrobat" combined with "Dropbox."
When issuing an RFP (Request for Proposal) for a new PACS, do not just ask "Does it have a viewer?" Ask these semantic questions to verify technical maturity:
Book a FREE demo now to experience Medicai first hand.
With PACS, medical images are accessible anytime, anywhere, allowing radiologists and physicians to review scans remotely, facilitating quicker diagnosis and treatment planning.
Unlike traditional film storage, PACS offers secure, cloud-based storage with encryption and backup capabilities, reducing the risk of data loss and ensuring compliance with regulatory standards like HIPAA (Health Insurance Portability and Accountability Act).
PACS integrates with Electronic Health Records (EHR) and Radiology Information Systems (RIS), allowing healthcare providers to access imaging data within patient records, improving workflow efficiency and reducing administrative burdens in critical sectors like Orthopedic, Cardiology or Oncology.
By eliminating manual film handling and automating image retrieval, PACS enables radiologists to interpret images more efficiently, reducing turnaround times and improving patient outcomes.
With digital storage, healthcare institutions save costs on film processing, physical storage, and transportation, while also optimizing physical space that would otherwise be used for film archives.
While PACS offers long-term cost savings, the initial investment can be significant, especially for smaller healthcare facilities. Cloud-based solutions, however, provide more affordable and scalable alternatives.
Given the sensitive nature of medical images, ensuring compliance with HIPAA and other data protection regulations is critical. PACS systems must have robust encryption, access controls, and backup mechanisms.
PACS security maps to administrative, physical, and technical safeguards under the HIPAA Security Rule. PACS technical safeguards include access control, audit controls, integrity controls, user authentication, and transmission security for ePHI.
PACS buying decisions get easier when security evidence is concrete, audit logs, least-privilege roles, encryption in transit and at rest, and tested incident response for ransomware scenarios.
Integrating PACS with existing hospital information systems (HIS), RIS, and EHR can be complex. Healthcare providers must ensure system compatibility and seamless data exchange to maximize efficiency.
Adopting a new PACS system requires adequate training for radiologists, technicians, and healthcare staff to ensure a smooth transition and efficient use of the technology.
PACS disaster recovery planning uses two metrics, RPO and RTO. PACS RPO defines acceptable data loss, and PACS RTO defines acceptable downtime for imaging operations.
PACS disaster recovery needs more than backups, because radiology operations need downtime workflows aligned with IT recovery steps.
Using our embeddable DICOM Viewer, you can easily view your imaging investigations anywhere online (on the web, in a mobile application). Your DICOM files are stored in your Medicai workspace, in a Medicai cloud PACS.
Artificial Intelligence (AI) is increasingly being integrated into PACS for automated image analysis, anomaly detection, and workflow optimization, improving diagnostic accuracy and efficiency.
Cloud-based PACS solutions are expected to dominate the market, offering greater scalability, cost-effectiveness, and real-time collaboration among healthcare professionals across different locations. However, the hybrid PACS architecture is gaining momentum as a futuristic solution.
Blockchain technology is being explored to improve data security, integrity, and interoperability in PACS systems, ensuring tamper-proof medical imaging records.
The growing demand for telemedicine is driving PACS evolution toward mobile access, allowing healthcare professionals to view and share images on mobile devices securely.
When selecting a PACS solution, healthcare organizations should consider the following:
PACS and RIS split imaging operations into two domains, PACS owns images and image distribution, RIS owns radiology workflow and scheduling. You use RIS to manage orders, appointments, modality worklists, and reporting workflows. You use PACS to store DICOM studies, retrieve priors, present images to radiologists, and deliver images to referrers and the EHR.
PACS-RIS integration succeeds when patient identifiers, accession numbers, and exam metadata match across systems. PACS workflow breaks fast when demographics drift, because the archive and the worklist stop agreeing on “who this study belongs to.”
PACS and VNA solve different storage problems, PACS optimizes clinical viewing and radiology workflow, VNA optimizes long-term, vendor-neutral retention. You need VNA when you want enterprise-wide imaging storage across multiple departments, multiple PACS, or multiple vendor migrations. You keep PACS when radiologists need fast hanging protocols, priors, diagnostic tools, and tightly integrated reading workflows.
PACS plus VNA becomes the standard pattern when an organization has more than 1 PACS instance, expects M&A consolidation, or plans a PACS replacement within 3 to 5 years.
Cloud PACS changes operations by moving core services, archive, compute, and distribution, into managed infrastructure instead of local hardware. You gain elastic storage and offsite resilience, and you trade local control for vendor operations, network dependency, and governance discipline.
Operational changes you will notice:
DICOM DIMSE and DICOMweb apply to different integration surfaces, DIMSE fits legacy modality and archive workflows, DICOMweb fits modern web viewers and API-first access. You use DICOM DIMSE when the modality talks Store, Query, Retrieve via classic association services, and the environment relies on established PACS networking patterns. You use DICOMweb when a zero-footprint viewer, cloud-native service, or external application needs HTTP-based query and retrieval.
DICOMweb usually maps to three service families:
Modality worklist prevents demographic errors by pushing a single, authoritative exam record into the modality before acquisition. You reduce “wrong patient” and “wrong exam” risk because technologists select scheduled items instead of typing names, MRNs, and procedure codes by hand. You reduce downstream clean-up because PACS receives consistent identifiers, accession numbers, and procedure metadata.
Modality worklist reliability depends on tight RIS integration and disciplined patient identity management. You get fewer split studies, fewer duplicates, and cleaner priors matching.
C-FIND and C-MOVE failures break PACS retrieval at the exact moment you need priors, comparisons, or cross-site reads. You see slow reads, missing prior exams, or a viewer that shows a study list that never opens. You trigger re-sends, manual exports, and shadow archives, which creates new data integrity problems.
Common breakpoints include mismatched AE Titles, ports, IP allowlists, routing rules, and patient ID inconsistency. Query/Retrieve stability matters because PACS reading speed depends on predictable retrieval, not heroic troubleshooting.
PACS retention decisions follow clinical risk, legal requirements, and storage economics, in that order. You keep studies long enough to support continuity of care, audits, and medico-legal needs. You align retention with jurisdiction, care setting, and specialty, then implement tiering so older studies move to cheaper storage without becoming “lost.”
PACS retention planning includes migration strategy, metadata integrity checks, and retrieval performance targets for older exams. You avoid forced, emergency migrations by planning retention and lifecycle before the archive reaches capacity.
PACS ransomware resilience depends on limiting blast radius and guaranteeing recovery, and immutable storage is the “cannot be changed or deleted” control that protects backups or archives during an attack. You use immutability to prevent attackers, or compromised admin accounts, from encrypting or deleting the recovery copy. You still need tested restore workflows, because immutability without restore speed produces long downtime.
PACS ransomware resilience needs a full stack:

PACS has transformed medical imaging by enhancing accessibility, efficiency, and security. As healthcare moves toward digital-first solutions, the integration of cloud-based PACS, AI, and telemedicine will play a critical role in shaping the future of radiology and diagnostic imaging.
Discover how Medicai's Cloud PACS can optimize your imaging workflows, enhance security, and improve patient care.
